Exercise during Pregnancy
After I found out that I had a high-risk pregnancy, one of the first questions that crossed my mind was, will I be able to continue to treat my patients despite the high level of physical exertion required? After consulting with the literature, I concluded that I am still physically capable of so much and that there are benefits from exercise for both me and my babies! In this review, we will go over the changes to expect in your body, how to incorporate physical activity and when to stop physical activity and seek support from a healthcare provider.
What are the physiological adaptations our body undergoes during pregnancy?
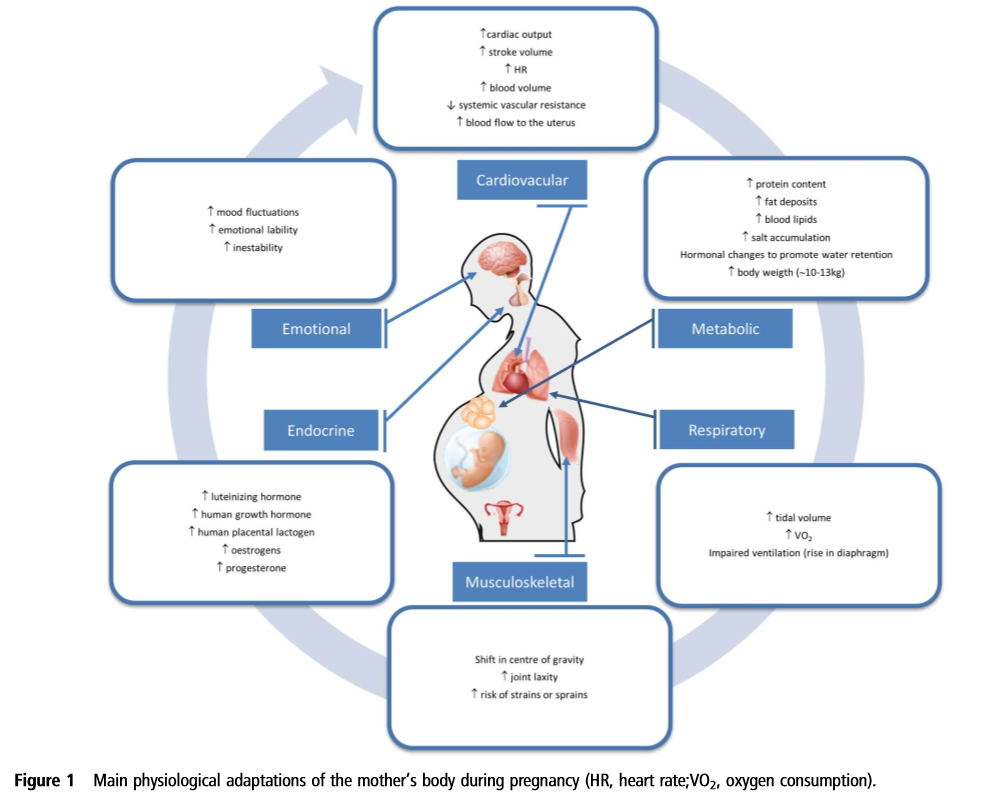
Each one of your body systems undergoes a massive shift to support the growth of your baby. Understandably, these changes will feel noticeable as you go about your daily activities and try to maintain your normal workout routine. Figure 1 (Barakat et al. 2015) shows cardiovascular, metabolic, respiratory, musculoskeletal, endocrine and emotional changes to expect throughout your pregnancy.
Each one of these changes will be felt in different ways and each pregnancy will differ in symptoms and the magnitude of those symptoms. In the context of exercise during pregnancy, some of the key changes which may impact you are respiratory changes and cardiovascular changes. For example, an increased baseline heart rate means the same amount of exercise pre-pregnancy will cause a more rapid rise in heart rate and a greater level of perceived exertion. Similarly, you may also feel shortness of breath due to a higher baseline level of oxygen uptake. All of this is to say, if you feel different or not quite yourself, this is totally normal and an important input into attuning your exercise to your new body.
What are the health benefits of physical activity during pregnancy?
The 2019 Canadian Guideline for Physical Activity throughout Pregnancy (Reference 1) found benefits to prenatal physical activity. Those who followed the guidelines experienced fewer newborn complications and greater maternal health benefits such as a decreased risk of pre-eclampsia, gestational hypertension, diabetes or excess weight gain and improved blood glucose. These mothers also experienced less instances of cesarean section or instrumental delivery, urinary incontinence, severe depression and lumbopelvic pain. Most importantly, higher levels of physical activity are not associated with negative outcomes such as miscarriage, stillbirth, neonatal death, preterm birth or labor and other common birth defects or complications. Figure 2 (Barakat et al. 2015) displays the physiological effects that exercise has on your body.
When is physical activity not safe for both me and my baby?
There may be instances, where exercise should be further moderated (relative contraindication) or even severely limited (absolute contraindications). Table 2 includes some examples of conditions which may require a more dramatic adjustment to your physical activity during pregnancy (Mottola et al. 2018). You may still be able to engage in light activity and if you have any concerns, always consult with your doctor.
What form of exercise is right for me and how do I measure the intensity?
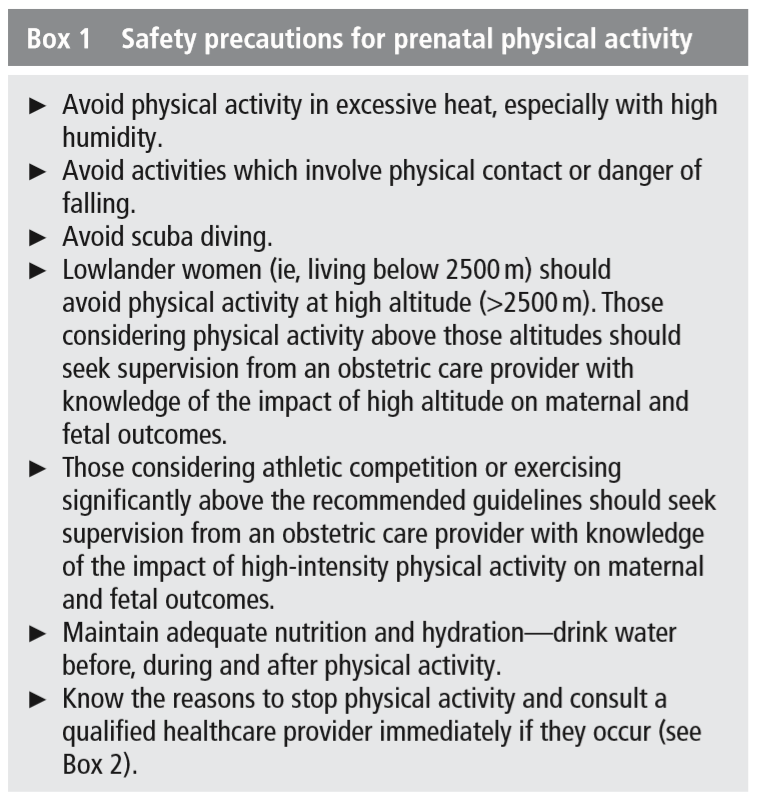
Most forms of exercise that you engaged in pre-pregnancy are still safe to continue during pregnancy. You may have to change and adapt the type of activity based on how you’re feeling or the level of risk such as engaging in contact sports. If you are new to exercise, don’t let that hinder you from starting a progressive program! You can consult your physical therapist in order to avoid sustaining an injury. Box 1 (Mottola et al. 2018) lists activities to avoid during this time to protect both you and your baby (for those not well versed in meters, 2,500 m = 8,200 feet).
If most forms of exercise are still ok during pregnancy, how much exercise is ideal? The UK Chief Medical Officers (Graphic) recommend 150 minutes of moderate activity each week which equates to around 20 minutes a day of activity such as walking, dedicated exercise, playing with children and other leisure activities.
One easy way to measure the intensity of your routine is to do the Talk Test. You know you are at a comfortable intensity if you’re able to maintain a conversation during physical activity and you should consider reducing the intensity of the exercise if this is not possible. If you have a heart rate monitor, you can try to keep your heart rate within the moderate intensity range for your age group, see Table 3 (Mottola et al. 2018).
When should I stop physical activity and consult a healthcare provider?
You know your body best and should lower intensity or cease activity if something doesn’t feel right. Box 2 (Mottola et al. 2018) shows when you should consult your doctor about your symptoms.
To summarize:
For most pregnancies, continuation of exercise has many benefits to both the mother and the baby
You may however, notice some bodily changes and need to adjust your exertion level of exercise routine
Target around 150 minutes of moderate intensity exercise a week
If you feel more severe symptoms such as dizziness, chest pain or excess shortness of breath, cease activity and consult a doctor if the conditions persist
References
Barakat R, et al. Exercise during pregnancy. A narrative review asking: what do we know? Br J Sports Med. 2015;49:1377–1381. doi:10.1136/bjsports-2015-094756
Mottola MF, et al. 2019 Canadian guideline for physical activity throughout pregnancy. Br J Sports Med. 2018;52:1339–1346. doi:10.1136/bjsports-2018-100056